Hi folks! AS you know the PHARM has an active bet on in countdown till 2020 with Dr Jo Deverill (@jodeverill), an emergency physician and one of the co-authors of the brilliant LITFL
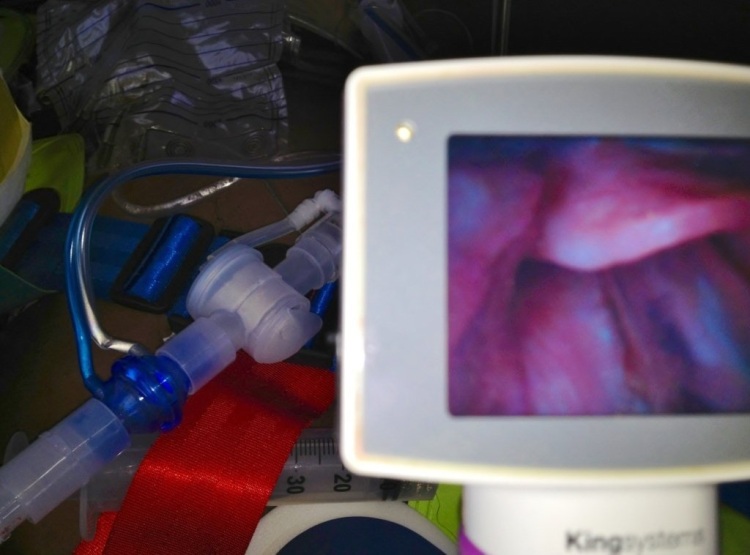
He bet me that by 2020 no Australian ED would still be using a direct laryngoscope per se ( CMAC style VL does not count by our rules!) and Video laryngoscopes would be the standard of care. I told him that would not happen, certainly not by 2020!
Anyway this week an American paper got published online that kinda supports Jo’s world view
One of its main authors Dr Sakles has published earlier this year, demonstrating the importance of first pass intubation success for minimising adverse events. No argument there as lots of previous work showing similar concept is true.
Some points to note about this latest paper seeming to support VL over DL:
– The paper excludes patients under 18yo
-VL devices used are Glidescope or CMAC
-Almost all the intubations in ED done in the paper are by EM residents grades 1-3
-First pass success is statistically greater in the VL group but no mention of overall ETI success is.
-Time to complete intubation is also not described. We know VL in previous studies has been shown to take significantly more time
-Difficult airway characteristics (DAC)are examined in the study and VL seems to improve 1st pass success in those with 1 or more DAC
-No complications of intubation are described such as hypoxia, hypotension, cardiac arrest
Take home messages:
1. This paper supports concept of using VL to intubate by EM residents to improve first pass success, especially for patients with 1 or more DAC
2. It seems confusing to have 2 different VL devices available to choose for EM residents to intubate with. I would not do that. Have 1 and get good at it!
3. I would report time to intubation completion and any airway related complications in future similar studies. The full picture is not described.
Bottom line : Video is killing the direct laryngoscope star..at least amongst EM residents in USA!
Interesting stuff Minh. A very different result to the paper in J Trauma Acute Care Surg http://www.ncbi.nlm.nih.gov/pubmed/23823612 which showed potential harm in an RCT from the use of VL in the ED.
This paper suggesting benefit is observational and it’s interesting to see how that affects what we see. Looking at the full paper there are a few things that stand out.
1. Very few (less than 2%) of intubations were done by attendings. These are trainees under supervision and therefore on the learning curve.
2. Of the airways predicted to be difficult the operators clearly chose to use VL. This is absolutely fine in my book as it makes sense I guess, but it does mean that the operators were choosing which device to use on the basis of the patient in front of them. Again, nothing wrong with that, but it may skew results. Why and how did some choose VL for predicted problems vs DL? We don’t know.
3. More patients were intubated VL as opposed to DL 1375 vs 1048 and that difference is almost totally accounted for by patients with predicted difficult airways.
4. It’s observational data and therefore likely to be full of all sorts of bias, some of which we can see and some which will be hidden away.
So, it’s interesting isn’t it, I’m really fascinated by how we use data for devices differently to drugs yet harm and benefits may result. VL vs DL is the topic of the moment but to be honest we could look at many other things. Here we have an RCT paper suggested that VL for everyone was a bad idea. This paper suggests that VL for some people is a good idea. So this new paper is welcome but still not definitive.
For what it’s worth I don’t think that ALL intubations will be done by VL in the next 6.3 years in the UK. Maybe in Queensland…………….
I agree with your other thoughts on the paper.
vb
S
Ref
http://stemlynsblog.org/2013/07/video-laryngoscopy-an-rct-in-trauma-st-emlyns/
Simon, an insightful commentary as always from you!
I think there is a lot of bias in this observational paper.
Sakles published an earlier paper on ED intubations and emphasised the importance of 1st pass success.
This paper continues along the same vein, mentioning only first pass success and that VL was better at that than DL. Saliently the time to intubation and complication rates are left out. The primary outcome described is only first pass success and also looking at patients with difficult airway features.
We know from the Dutton RCT you cite that VL there was shown to take longer and there was a trend to worse mortality in the TBI subgroup.
on a side note RCT in airway management is very tricky to do. You are always facing the problem of getting standardised group of providers so that what you end up studying is not so much differences between airway devices, but differences between airway providers! Thats why many airway studies are done by a single provider or a very small group so as to seek to standardise the provider variable!
An observational ED study using several grades of EM resident is going to have trouble controlling for skill variability and device bias.
The odd factor I found in this study was that they allowed the choice between two quite different VL systems : Glidescope vs CMAC.
In effect that weights the study results in the VL camp favour! if tube done successfully with CMAC, that still is counted as VL..even if DL technique was done ( as far as I can tell by reading the paper!)
Thanks for discussing this, Minh. Sakles has multiple publications on this topic looking at all sorts of different things with VL. The one thing I always come back to with this stuff is that in every paper I’ve seen, the rescue technique for failed VL was DL. You still need to be good at DL regardless of what you are using first or most. Also, the VL devices are not all equivalent. They require different techniques when using them so you really need to be familiar with your device. Glidescope now has a handle like CMAC that you can use as both DL and VL which is wonderful for training purposes.
At the end of the day, I think you need to be great with epiglottoscopy and everything else will fall into place.